Article content
Nearly a third of Americans are obese and annual treatment costs amount to $ 147 billion.
According to the CDC (the U.S. Centers for Disease Control and Prevention) throughout 2014 obesity did not fall below 20% across the entire United States.
These figures differ significantly from the values the CDC reported for 1990. At that time, in no U.S. state did obesity exceed 15%.
The rise in obesity is attributed to various factors — from increased energy intake that your body does not need, lack of physical activity to consuming the wrong types of foods.
The human body does not burn carbohydrates efficiently and it often happens that already after a few hours we feel hungry again. Alcohol is also a carbohydrate. Studies deliver conflicting results — some recommend a glass of wine with dinner, while others recommend complete abstinence.
Some inconsistencies may be related to the amount of alcohol that participants drank during the individual studies. The results of the most recent study say that alcohol is linked to the development of up to seven types of cancer.
The risk of developing cancer increases with alcohol consumption
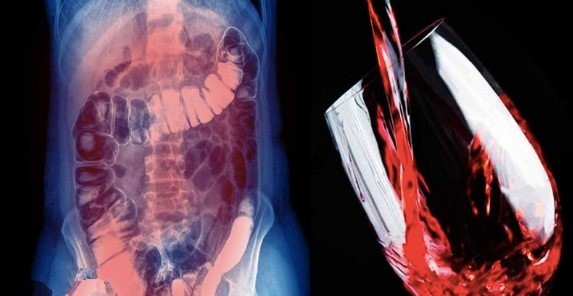
The journal Addiction published research that provided significant evidence that alcohol is commonly associated with cancers of the rectum, liver, colon, esophagus, oropharynx (part of the pharynx in the mouth), larynx and, in women, the breast.
An epidemiological study suggests that alcohol contributes to 5.8% of cancer deaths worldwide. The research did not establish a biological causal mechanism between alcohol consumption and cancer development in these seven organs, although the researchers felt the following:
“To deduce that alcohol is the cause is possible even without confirming specific biological mechanisms by which alcohol increases the incidence of each type of cancer.”
The percentage of total deaths related to alcohol and cancer increased by 62% over the last 12 years, from 3.6% in 2003 to 5.8% in 2015.
Such an increase may also be the result of various other factors affecting the lives of people in whom cancer development was caused by alcohol consumption. Such factors may include poor diet, lack of exercise or poor sleep quality.
To establish a causal relationship between alcohol drinking and cancer development, participants would have to be randomly assigned to two groups.
Throughout the participants’ lives one group would drink alcohol and the other would abstain. Instead of such a division researchers examined a huge amount of epidemiological data that are closely related to alcohol consumption and cancer occurrence.
Another study even found a link between moderate alcohol consumption and the development of the mentioned types of cancer. Researchers followed nearly 136,000 cases of men and women for more than 30 years.
They found that among smokers (including those who quit smoking) the incidence of alcohol-related cancers was higher than among people who never smoked.
This study confirmed that smoking significantly contributes to the development of the types of cancer associated with alcohol consumption.
Breast cancer recurrence associated with alcohol consumption
The American Cancer Society warns that even a few alcoholic drinks per week increase the risk of developing breast cancer. The risk is higher in women who have a low folate level.
Other research links breast cancer recurrence with alcohol consumption.
Both of these connections stem from alcohol’s ability to increase estrogen levels. Alcohol also affects male hormones.
Chronic alcohol consumption in men is associated with testicular dysfunction and infertility. Feminine symptoms in men suggest that alcohol may contain biologically active phytoestrogens.
Phytoestrogens occur in some plants such as soy, flax seeds, wheat, lentils and sesame seeds.
By their composition these phytoestrogens resemble the estrogen produced by the human body and freely bind to estrogen receptors.
Although studies from Asia associate consumption of soy products with a reduced incidence of breast cancer, these results were not confirmed in the USA. The difference may lie in the different types and amounts of plant products containing phytoestrogen consumed.
Increased estrogen levels in the body are also linked to an increased rate of cell growth, which plays an important role in the development and progression of prostate cancer and some types of breast cancer.
Each of these effects was observed in people who drink alcohol in small amounts. This means that even drinking alcohol in small quantities does not exclude the development of breast cancer in women and prostate cancer in men.
Preliminary findings from these studies suggest that if you have been diagnosed with breast or prostate cancer (and especially if you are overweight or postmenopausal), it would be advisable to reduce or eliminate alcohol intake.
Colon cancer increasingly affects people under 50
Colon cancer is also linked to alcohol consumption. A study published in the journal Cancer found that every seventh person diagnosed with colon cancer was under 50 years old.
According to current recommendations screening for colon cancer should begin in people who have reached 50 years of age.
Doctors usually diagnose colon cancer in younger people only after symptoms of the disease appear, such as bowel obstruction, blood in the stool and anemia.
The research clearly confirmed the association between colon cancer and alcohol consumption. The International Agency for Research on Cancer (IARC) in 1988 classified alcohol as a Group 1 carcinogen.
According to IARC, Group 1 carcinogens are the highest-risk category because they are proven carcinogens.
This is clear evidence that alcohol really causes cancer. A 2011 study found that 4% of cancer cases in the United Kingdom can be attributed to alcohol consumption.
In cases associated with alcohol consumption, colorectal cancer was the most frequently represented.
A study published in 2004 in the journal Nutrition and Cancer found that the risk of developing colon cancer increased by 70% in participants who drank one or more alcoholic drinks per day.
The type of alcohol did not play a role. In other words, it did not matter whether participants consumed beer, wine or spirits — the increased risk was the same.
Another study followed patients who had previously had a specific type of colorectal polyp called an adenoma.
Researchers found that alcohol intake significantly increases the risk of developing another colorectal adenoma, thereby increasing the risk of colorectal carcinoma.
The risk begins in the mouth
The development of alcohol-related cancer is strongly contributed to by the effect of acetaldehyde on our DNA.
Acetaldehyde is a metabolite of alcohol oxidation that damages DNA and prevents the body from repairing this damage. It is most closely associated with cancers of the pharynx, larynx, esophagus, mouth and liver.
Alcohol is broken down in the liver, producing acetaldehyde. This substance causes faster growth of liver cells and sometimes leads to their genetic mutation.
This process can lead to the development of liver cancer. Alcohol can also be broken down by bacteria that live in the mouth and intestines.
This increases the amount of acetaldehyde to which your mouth, pharynx, larynx and esophagus are exposed, increases damage to cellular DNA and the risk of oral cancers.
Other sources of acetaldehyde are tobacco and flavoring agents. It has been found that a significant direct source is alcohol.
Researchers, in an effort to reduce cancer risk, urge public health measures to be taken and to reduce the acetaldehyde content in alcohol.
Sugar contributes most to disease development
It thus increases the risk of high blood sugar levels and insulin resistance.
Since it has no nutritional value, we can view it as empty calories. Empty calories are a problem that contributes to the global rise in obesity.
Alcohol is one of the carbohydrate-rich foods that doubles the risk of developing cancer by exposing you to acetaldehyde and at the same time increases the risk of obesity.
A 2013 study by research institute Credit Suisse titled Sugar: Consumption at a Crossroads found that 40% of total U.S. healthcare expenditures go to treating diseases that arise from excessive sugar consumption.
Recent research confirmed the association between cancer in adults over 30 and high BMI (overweight to obesity).
25% of cancer cases in 2012 were directly caused by increases in BMI from 1992.
The metabolism of sugars and cancer cells both require an anaerobic environment. Many types of cancer cannot produce enough energy without sugar to survive. When you reduce carbohydrate intake (except for fiber), cancer cells literally starve to death.
One can of beer contains up to 13 g of carbohydrates, one glass of wine (150 ml) has 4 g and one cocktail (150 ml) has 10 g of carbohydrates.
As seen in these examples, even one glass of alcohol a day can significantly increase sugar intake and provide the body with no nutrients. In this way it contributes to the development of obesity, insulin resistance and cancer.
Nutritional ketosis in cancer treatment
Although commonly stated otherwise, nuclear genetic defects do not cause cancer. First there is damage to the mitochondria, which later results in the triggering of nuclear genetic mutations.
Nutritional ketosis, which requires a diet high in high-quality healthy fats and significantly limits the intake of pure carbohydrates, supports proper mitochondrial function.
Healthy mitochondria effectively burn fat because it is a much more suitable fuel than sugar. With nutritional ketosis you can prevent most types of cancer, or even treat them.